For more than two decades, cancer death rates have declined steadily in the United States.
The
Cancer death rates also decreased across different racial and ethnic populations, according to the report, published on April 21 in the journal
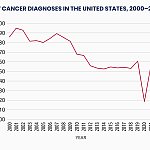
The report also shows a drop in cancer diagnoses among males from 2001 through 2013 before stabilizing through 2021.
Among women, however, there were yearly increases in cancer diagnoses from 2003 to 2021.
Cancers associated with obesity are also on the rise. These include female breast, uterus, colorectal, pancreas, kidney, and liver cancers.
However, the report notes that these trends in death rates and diagnoses were interrupted during the COVID-19 pandemic, likely due to barriers to medical care and missed screenings. This gap in the data could lead to an uptick in cancers diagnosed at later stages in the years to come, the researchers explained.
“The magnitude of the 2020 decline was similar across states, despite variations in COVID-19 policy restrictions,” an
“These findings underscore the importance of providing access to health care, even during public health emergencies, to ensure the timely diagnosis of cancer.”
A decline in death rates from cancer is considered the gold standard for measuring progress made in diagnosis and treatment.
The researchers attribute some of the decline in cancer deaths to reduced incidences and death rates from lung cancer and other smoking-related cancers.
Jack Jacoub, MD, board certified medical oncologist and medical director of MemorialCare Cancer Institute at Orange Coast and Saddleback Medical Centers in Orange County, CA, agreed.
“I suspect the strong interaction of smoking cessation and decline in smoking-related cancers significantly influences this finding in men — more men smoked and have since stopped,” he told Healthline.
Jacoub added that improved screening programs and access help detect cancer at earlier stages and improve treatment outcomes and survival rates.
He noted that improved patient-specific factors, such as healthier lifestyles, including smoking cessation, exercise, weight control, and limiting alcohol consumption, are perhaps more significant.
“[These] all theoretically improve tolerability to and possibly benefit from cancer therapy and improved therapeutics,” Jacoub said.
Anton Bilchik, MD, PhD, surgical oncologist, chief of medicine, and director of the Gastrointestinal and Hepatobiliary Program at Providence Saint John’s Cancer Institute in Santa Monica, CA, echoed Jacoub’s remarks.
“We have better screening and better understanding of cancer prevention. We recommend avoiding risk factors such as obesity, processed food, and inactivity,” Bilchik told Healthline.
“We’re learning that all these factors are important, even as a child, and that’s partly relevant to cancers that are increasing in young people, such as colorectal cancer.”
“While overall incidences are declining and overall outcomes are better, we are seeing some, like colorectal cancer in young people, going up, and it’s the leading cause of cancer-related deaths in people under 50 and second among women.”
While cancer death rates decreased, the report highlights a gradual increase in diagnoses among females, particularly breast and uterine cancers.
As female cancer rates increase, the report also highlights that women in racial minority and ethnic groups are disproportionately affected. From 2017 to 2021 (excluding 2020), cancer diagnoses were highest among American Indian and Alaska Native women.
Jacoub and Bilchik noted some factors contributing to these disparities may include:
“Improvement can be achieved [through] education and improving access for all patients,” Jacoub said.
Bilchik said the disparities in female cancer rates were “alarming” and that more work needs to be done to address socioeconomic differences and improve access and screening in areas with limited access to healthcare.
“Women who have less access to healthcare have a large increase in certain cancers, such as breast and uterine cancer, compared to those who have access to screening,” Bilchik said.
Screening for cancer is crucial, particularly for those facing higher risks.
Routine screening can diagnose cancer in its earlier stages and at the most curable point in time.
Jacoub recommended that women and other at-risk individuals practice the following healthy habits for cancer prevention:
Bilchik emphasized the importance of a healthy gut microbiome to help fight inflammation and maintain overall health.
“There is a lot of data now that we carry these trillions of bacteria and viruses in our body known as the microbiome, and it’s important to eat a healthy, balanced diet to enhance healthy bacteria and viruses in our body,” he said.
“Processed foods or too much alcohol can have a negative impact on the microbiome, which has been shown to have an impact on our immune system. When the microbiome is not balanced, there’s a higher risk of cancer.”