New research suggests the small cardiovascular risks associated with attention deficit hyperactivity disorder (ADHD) medications like methylphenidate, bupropion, and lisdexamfetamine do not outweigh their mental health benefits.
The study, published on April 6 in
The findings show relatively small increases in pulse, blood pressure, and electrocardiogram (ECG) readings in those taking ADHD stimulants. Increases were also observed in those taking noradrenaline reuptake inhibitors, a type of antidepressant. A third type of medication, alpha agonists, showed the inverse: a decrease in heart rate and blood pressure.
The authors concluded that while ADHD medications tend to raise heart health indicators like blood pressure and pulse, the current best practice of patient monitoring can lead to successful health outcomes.
Cheng-Han Chen, MD, an interventional cardiologist and the medical director of the Structural Heart Program at MemorialCare Saddleback Medical Center in California, said the research reaffirms that those taking ADHD-related medications should be screened for cardiovascular risk factors, such as a family history of heart disease.
Chen wasn’t involved in the study but told Healthline that given the age range for many of the studies focused on youth, it’s important to help young people understand what a heart-healthy lifestyle looks like.
“As of now, this research says there is not a dramatic change in cardiovascular risks, but it’s something that probably should be tracked over the long term to look at long-term outcomes,” Chen said.
Anoop Singh, MD, a general psychiatrist and regional medical director for Mindpath Health in California, agreed that the findings are reassuring for patients and clinicians. Singh wasn’t involved in the study.
“If anything, it reinforces… that mental health practitioners or psychiatrists should continue to closely follow the current clinical guidelines, which include monitoring of the blood pressure and the pulse before and during the treatment with ADHD medications,” Singh told Healthline.
“So, no surprises. The study did, in fact, basically extend the findings of previous similar studies.”
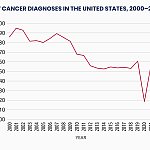
There has been a significant increase in the number of people diagnosed with ADHD in the last decade, according to the Centers for Disease Control and Prevention (CDC).
While research shows this increase is likely a combination of public and medical awareness, some medications used to treat ADHD, like Ritalin, have also been stigmatized.
When used appropriately, ADHD medications lead to better mental health outcomes and improved quality of life. A 2019 analysis found that ADHD medication led to lowered instances of injuries and substance use disorder, although there were some limitations to these findings.
Still, as with any medication, prescription or over-the-counter, there are risks.
“Even an over-the-counter Sudafed carries the risk of causing some increase in blood pressure and heart rate,” Singh noted.
“However, when you are contemplating [the] use of these medications in a medical setting, we have to at least allow some level of confidence to be placed in the fact that, given that a treatment intervention is being suggested as a medical treatment, there would be an appropriate process of evaluating and monitoring for side effects,” he said.
When cardiologists screen people diagnosed with ADHD, Chen said they look for several factors before a patient is prescribed medication.
“Just like any other person, we would screen for cardiovascular risk factors such as high blood pressure, high cholesterol, [and] diabetes,” Chen said.
“We would counsel the patients the same way about maintaining a healthy lifestyle, including a heart-healthy diet, exercise, avoiding smoking, avoiding drinking, getting good quality sleep.”
One challenge for researchers is that none of the studies analyzed included follow up after 26 weeks with most looking at patients over 12 weeks.
Singh noted this was a common issue, not just in psychiatry but across medicine.
“There is always going to be some want of more, better, longer term, studies to give us more data,” he said.
“And because medicine, or at least Western medicine these days, is so evidence-informed, we are always hungry for more evidence.”
In a
Pliszka noted this could include hourly checks of cardiovascular indicators for one day every six months. Another path forward, he wrote, could be using machine learning to help comb through broader databases for relevant information.
The study authors pointed out that long term data was lacking and that their findings could not account for possible individualized cardiac health risk factors, such as a family history of heart disease.
They cautioned that just because increases in measures like blood pressure and pulse were small on average, it didn’t mean that for some people, they could be higher and require medical intervention.